Dehydrated Skin
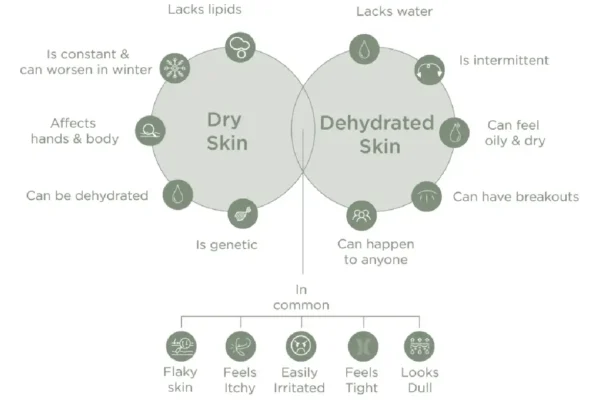
It should be noted that there is a clear difference between dehydrated skin and dry skin.
DIFFERENCE BETWEEN DRY & DEHYDRATED SKIN
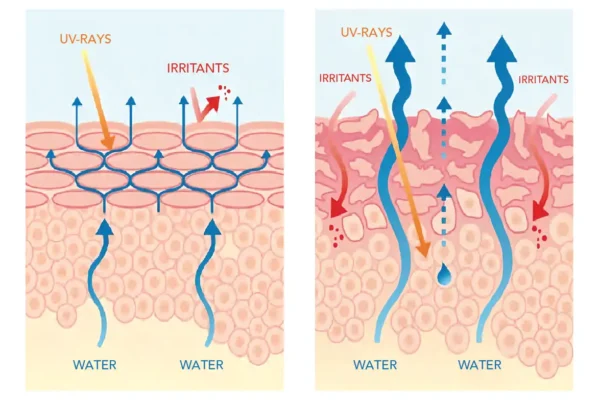
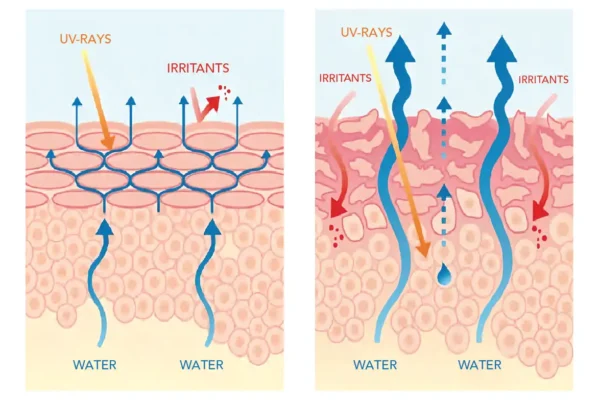
When the skin lacks water, it can no longer fulfill its function as a protective barrier against external aggressions and encounters greater difficulties in the face of mechanical movements; stretching, tugging and small wrinkles begin to appear.
A quick way to determine if your skin is dehydrated is the pinch test: pinch your skin and see if it takes a long time to return to its original shape. If that is the case, you have dehydrated skin. To treat skin dehydration, we must first understand why the skin is dehydrated in the first place.

Approximately 65% of an adult’s total body weight is water and of that total water weight, 15% is present in the skin.
Water therefore plays an essential role in maintaining the health of the skin. The skin, which covers the entire human body, acts as a reservoir on which other organs rely for their water needs.
It allows for interaction between the body and the external environment as water moves from the dermis to the surface.
This flow of water is called transepidermal water loss (TEWL).
This process is normally protected by a hydrolipidic film on the stratum corneum (outermost layer of the epidermis) that slows down the evaporation process: this is the physiological barrier.
If there is a problem with this physiological barrier, water loss through evaporation accelerates, making the skin excessively dry.
In addition to an inherent problem with the hydrolipidic layer, other external
Environmental factors: cold weather, wind, winter season, pollution, UV rays…
Emotional factors: stress, fatigue…
Lifestyle factors: smoking, alcohol…
Certain medications: anti-acne treatments, anti-cholesterol medications
Certain cosmetic products: aggressive, scouring or drying products.
Water regulation in the skin
The skin is 70% water and 75% of this water is located
deep in the dermis where it plays a key role in the skin’s
barrier effect against the elements.
There are 2 types of water in the epidermis
- STATIC OR FIXED WATER
- DYNAMIC OR CIRCULATING WATER
Water regulation is the balance between static and dynamic water. This balance provides both the physical integrity and the functional properties of the skin.
3 IMPORTANT COMPONENTS PARTICIPATE IN WATER REGULATION
- Natural Moisturizing Factors (NMF) NMFs are molecules produced by the body that bind to water in the skin and prevent its evaporation. The most common NMFs present on the skin are urea and lactic acid. Recently, cosmetic products have begun to incorporate several ingredients that have the same properties, such as glycerin, to achieve the same effect.
- Lipids of the stratum corneum
- Aquaporins
To improve your skin’s hydration, reduce water evaporation as much as possible and repair the integrity of the skin barrier:
Stay hydrated by drinking at least 1.5 liters of water per day (unless otherwise advised by your doctor)
Maintain a healthy indoor atmosphere by avoiding air-conditioned (due to dry air) or extremely heated (due to hot air) rooms that accelerate
evaporation
Avoid exposing your skin to intense cold or the harmful effects of UV rays or protect yourself when faced with these conditions
Wash your face twice a day, in the morning to get rid of the excess sebum secreted by your skin during the night and in the evening to remove oils and toxins that adhere to your skin from the outside environment
Apply an emollient to repair and protect the skin barrier and reduce tightness.
Choose skin-friendly skin care products and use rehydrating, non-detergent cleansers
Consult your dermatologist, physician or pharmacist to choose the right product for your skin. If, after using a cosmetic product, your condition does not improve or gets worse, consult your dermatologist or pharmacist.
Related Products
Dry Skin
Dry skin is very uncomfortable and sometimes painful, with cracking and sometimes even bleeding. People with dry skin feel uncomfortable in their own skin.
Symptoms of dry skin:
- Dry skin is a physiological condition in which the skin barrier is weakened and can no longer protect the body from external aggressors. The skin does not produce lipids or oils to lubricate itself
- This results in a feeling of discomfort, accompanied by tightness, stiffness and flaky skin. Under these conditions, the skin loses its barrier function
- Dry skin, also known as xerosis, is a breeding ground for eczema, especially in the form of dry patches (pityriasis alba).
Instead of smooth skin, the skin is tight and even rough - These symptoms can sometimes be accompanied by itching and burning sensations

Dry skin: the person feels a temporary discomfort, slight but infrequent tightness with a slight scaling
Very dry skin: the person feels discomfort and significant tightness, intense desquamation, cracks, chapping
A hydrolipidic film formed mainly from a combination of water and sebum generally protect the surface of healthy skin.
This film makes the skin waterproof, protects it from external aggressions and reduces water loss. When the top layer of the epidermis does not have a good balance of water and lipids, it can no longer effectively fulfill its role as a barrier and becomes uncomfortable to varying degrees, as we have seen above Skin dryness is linked to the genetics of each individual, however, there are external factors that can trigger or aggravate it:
- Climate, environmental conditions (heat wave, cold)
- Medical treatments (such as acne medication)
- Skin diseases or general illnesses: diabetes, psoriasis, atopic dermatitis, eczema, thyroid hormone imbalances, nutritional deficiencies...

- Avoid excessive heat
- Drink enough water (1.5 liters of water per day) to stay hydrated (Unless otherwise directed by your doctor)
- Wash your face with an appropriate soap free cleanser that respects the skin’s hydrolipidic film
- Apply a moisturizing cream to soothe and protect the skin. A moisturizing or emollient cream is a product that fills the cracks in the skin
- Consult your dermatologist, doctor or pharmacist to choose the right product for your skin. If, after using a cosmetic product, your condition does not improve or gets worse, consult your dermatologist or pharmacist
Dry skin is characterized by significant, painful cracking. The daily application of an emollient can reduce the cracks.
In theory, putting an emollient on your skin may seem like an easy step, but it is overly important in order to get quick relief
An emollient should be applied to a large area of the skin for best results, and it should not be localized only to the area affected by the cracks, as micro-cracks invisible to the naked eye may develop.
The application of an emollient is much easier when the skin is slightly damp after a shower.
Ideally, it should be used twice a day, once in the morning and once in the evening, and incorporated into a daily routine so as not to be forgotten.
Related Products
Normal Skin
Some people are fortunate enough to have what is called normal skin. Normal skin is skin that is generally problem-free, but in some cases can become dry or oily, depending on environmental conditions and seasonal weather changes. It can also manifest itself as combination skin when irritated
The best way to care for normal skin is to use morning and evening:
- a gentle, soap-free facial cleanser that respects the skin’s hydrolipidic film
- a moisturizing serum with hyaluronic acid (HYDRA PLUMP)
- a stabilized vitamin C-based antioxidant serum will help keep your skin in top shape and defend it against oxidative stress (BOOST C)
- an eye contour cream (BOOST EYE)
- a nourishing day and night cream (BOOST LIFT)
- a sunscreen with a minimum SPF30
- an anti-aging retinol serum
Even if your skin is normal, young and healthy at the moment, you need to consider the effects of the environmental damage it is experiencing daily. Taking care of your skin should start at a young age to mitigate the cumulative effect of sun exposure, environmental damage, and age changes
As the saying goes, ” an ounce of prevention is worth a pound of cure “. Consult your dermatologist, doctor or pharmacist to choose the right product for your skin. If, after using a cosmetic product, your condition does not improve or gets worse, consult your dermatologist or pharmacist

Related Products
COMBINATION AND OILY SKIN
Combination and oily skin is more prone to blemishes than other skin types.
Puberty, excess sebum secretion, clogged pores and bacterial overgrowth cause skin blemishes to appear.
These imperfections may disappear on their own as sebum production decreases and the skin dries out in adulthood, but they can also persist beyond adolescence into adulthood.
In the case of combination skin, the majority of skin imperfections are located in an area of the face called the T-zone. This area includes the forehead, nose and chin, forming a T, hence the name. Other areas of the body may have a combination of normal or dry skin in some cases.
Acne breakouts are more common during adolescence in certain areas of the body such as the face, chest and back because sex hormones cause an increase in the production and secretion of sebum. At the age of 14, the skin starts to become oilier, which leads to the appearance of acne pimples in these areas. On average, 80% of teenagers have acne in both age groups and the condition can persist into adulthood. In some cases, acne can affect newborns due to their mother’s hormones that are present during childbirth. This type of acne usually resolves itself. Acne can clear up on its own as individuals begin to transition into adulthood, but it can still occur in adults especially if it has not been treated.

- Hyperseborrhea: Hyperseborrhea is an excessive production and secretion of sebum caused by the hormonal changes of puberty. Sebum gives the skin a shiny, oily appearance. There is an excess of sebum quantity as well as a change in the quality of sebum that is controlled by these hormones, the person’s diet and environment. The sebum of oily skin is generally thicker than normal sebum and drains with greater difficulty from the pores, which increases the risk of clogging them, hence the need for daily cleaning.
Using a gentle cleanser for oily skin such as BECLEAN will remove excess oil without drying out the skin. After cleansing your skin of excess sebum, you need to prevent the sebum from re-clogging the pores.
Applying a sebum-regulating product such as BECLEAN MAT helps to reduce sebum secretion, making the skin less shiny and oily and preventing the problems already mentioned. - Bacterial proliferation: sebum is a good nutrient for facial bacteria. With excess sebum, the face becomes a breeding ground for bacteria, including Propionibacterium acnes, which is normally present on the face in normal quantities, but whose numbers increase in the presence of sebum. The increase in the number of these bacteria will lead to inflammation on the surface of the skin and the formation of pimples, comedones and acne pustules. A good measure to avoid this bacterial proliferation is to control and reduce the quantity of sebum from which the bacteria benefit.
- Hyperkeratinization: this is the excessive renewal of skin cells that leads to a greater number of dead cells. The massive excretion of skin cells blocks the pores of the follicular canal and prevents the sebum from being secreted on the skin’s surface. In addition, the cellular debris (proteins and lipids) provides more nutrients for bacteria. The blocked comedo, which contains sebum, dead cells and bacteria, will fester and turn first into a papule, then into a pustule. It is therefore necessary to exfoliate the skin to avoid the accumulation of dead cells, which are a source of energy for bacteria and constitute the pore plug.
The presence of silica in BECLEAN MAT and silica microbeads in BECLEAN will help to exfoliate the skin properly and prevent pores from clogging. Best of all, silica is a gentle abrasive agent which, in turn, unclogs pores and reduces the appearance of acne.
In addition to the common causes of acne in both sexes, women are more likely to develop acne as adults than men for the following reasons:
- Genetics
- Sun exposure
- Use of inappropriate cosmetics
- Use of unknown skin irritants
- Smoking, as smokers are more likely to get acne than non-smokers.
- Medication: oral contraceptives and hormone therapy cause acne to appear.
- Hormonal fluctuations: after the age of 30, a late-onset hormonal acne outbreak begins to appear around the jawline and neck in women.
As we age, the skin becomes dry and therefore less oily. However, adult acne can still develop in the form of pustules and comedones. These skin lesions can be treated, but the treatment of adult acne is different from that of adolescent acne.

- Avoid touching your skin blemishes: this will only exacerbate your
acne, as you are introducing foreign pathogens to an inflamed skin
surface, which infects it and turns those papules into pustules at the risk of acne scarring. - Avoid sun exposure: Although you may be tempted to use tanning to hide your skin imperfections, the opposite effect will happen and an acne flare-up will occur at the end of the summer. The sun’s rays have a largely negative effect on acne-prone skin. The sun’s UV rays eliminate the bacteria responsible for acne, which explains why acne disappears at first. But the sun is a double-edged sword because it stimulates the secretion of sebum, the oily substance involved in the process leading to acne. The sun’s rays also cause dryness and thickening of the skin, which are part of the problem of oily skin and will worsen your condition.
- Follow your dermatologist’s treatment: Apply a topical treatment to your face once or twice a day that is specifically designed for combination to oily skin and approved by your dermatologist. Results begin to appear after 4-6 weeks of treatment. Some topical or oral treatments may dry out your skin. You should discuss this concern with your dermatologist, who will help you use an adjunctive treatment to improve your skin’s moisture level.
- Wash your face with an appropriate soap-free cleanser that respects the skin’s hydrolipidic film.
- Consult your dermatologist, doctor or pharmacist to choose the right product for your skin. If, after using a cosmetic product, your condition does not improve or worsens, consult your dermatologist or pharmacist.